Recurrent airway obstruction (RAO) is a common disease in horses. It used to be known as COPD, but as the pathophysiological mechanisms are more similar to human asthma than to human COPD, the disease is called RAO since 2001.
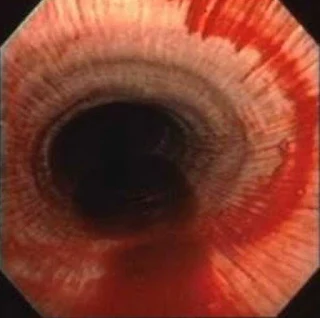
The disease is not always clinically present, but after environmental challenge, horses show moderate to severe expiratory dyspnoea, next to nasal discharge and cough. The onset of the disease is caused by inhalation of environmental allergens, especially hay dust, that cause severe bronchospasm and in addition hypersecretion. The mucosa becomes swollen while accumulated mucous secretions further contribute to airway narrowing.
During remission, clinical symptoms may subside completely, but
a residual inflammation of the airways and a hyperreactivity of the bronchi to
nebulized histamine still remain present. A low degree of alveolar emphysema
may develop as well, caused by frequent episodes of air trapping. In the past,
severe end-stage emphysema was often diagnosed, but today this is rather
uncommon and only sporadically occurs in old horses after many years of illness.
The commonly accepted allergens that cause or provoke an exacerbation of RAO
are especially spores of Aspergillus fumigatus and Fusarium spp.
Although the RAO shares many similarities with human asthma, an accumulation of eosinophils in the BALF at exacerbation has never been reported. An asthma attack in humans is characterized by an early-phase response of bronchoconstriction, occurring within minutes of exposure to inhaled allergens. This phase is followed by a late asthmatic response with the continuation of airway obstruction and the development of airway inflammation. Mast cells play an important role in this early asthmatic response.
The activation of mast cells
after inhaling allergen results in the release of mast cell mediators, including
histamine, tryptase, chymase, cysteinyl-leukotrines, and prostaglandin D2.
These mediators induce airway smooth muscle contraction, clinically referred to
as early-phase asthmatic response. Mast cells also release proinflammatory
cytokines that, together with other mast cell mediators, have the potential to
induce the influx of neutrophil and eosinophil granulocytes and the
bronchoconstriction that are involved in the late-phase asthmatic response.
Activation of another type of mast cell receptors can also induce mast cell degranulation or amplify the Fc-RI mediated mast cell activation.
In horses suffering RAO, such an early-phase response seems not to appear, whereas in healthy horses the early phase response does appear. This early-phase response may be a protective mechanism to decrease the dose of organic dust reaching the peripheral airways . Apparently, in the horse with RAO, this protective mechanism has been lost and only the late-phase response will develop. The time of exposure to dust plays a determining role, as was shown by studies with exposure to hay and straw for 5 hours. This challenge caused an increase of histamine concentrations in BALF of RAO-affected horses, but not in control horses. In contrast, exposure of only 30 minutes to hay and straw did not result in a significant increase in BALF histamine concentration of RAO horses.
A study showed that exposure to hay dust of at least
1 hour is needed to provoke signs. The evidence that the duration of exposure to organic dust must be longer than 1 hour well proved. There is the opinion that the necessary exposure to provoking clinical
signs of airway obstruction varies from hours to days in RAO-affected horses.
The
role of IgE-mediated events in RAO is still puzzling. Serum IgE levels against
fungal spores in RAO horses were significantly higher than in healthy horses,
but counts of IgE receptor-bearing cell in BALF were not significantly
different between healthy and RAO-affected horses. T-helper cell response of type 2 responsible for the
clinical signs, similar to human allergic asthma. However, their results are in
contradiction with results of other research groups who could not find
differences in lymphocyte cytokine expression patterns in cases with
exacerbation of RAO compared to a control group.
The
diagnosis of RAO is made if at least 2 of the following criteria are met:
expiratory dyspnoea resulting in a maximal intrapleural pressure difference
(ΔpPlmax) > 10 mm H2O before provocation or > 15 mm H2O
after provocation with dust or by bad housing conditions. Any differential
granulocyte count of > 10% in BALF is an indication for RAO. If symptoms can
be ameliorated with bronchodilator treatment, the diagnosis is totally
established. In some severe cases, the arterial PaO2 may be
below 82 mmHg. After provocation with hay dust, RAO patients may reach equally
low arterial oxygen levels too. Keeping the animals for 24 hours on pasture
will quickly reduce clinical symptoms to a subclinical level.
The visible morphological changes are primarily located in the small airways and spread reactively to the alveoli and major air passages. Lesions may be focally, but functional changes may manifest themselves well throughout the bronchial tree. Bronchial lumina may contain a variable amount of exudate and may be plugged with debris. The epithelium is infiltrated with inflammatory cells, mainly neutrophil granulocytes. Furthermore, epithelial desquamation, necrosis, hyperplasia, and non-purulent peribronchial infiltrates may be seen. Fibrosing peribronchitis spreading in neighboring alveolar septa was reported in severely diseased animals The extent of these changes in the bronchioles is related to a decrease in lung function, but changes may be distinctly focal in nature.
Especially the function of Clara cells is important for the integrity of the bronchioles.
Mildly diseased animals show loss of Clara cell granules next to goblet cell
metaplasia even before inflammatory changes occur in the bronchioles. This
together with the ultrastructural alterations found by supports the idea of
the damaging effects of dust and LPS. In severely affected horses Clara cells
are replaced by highly vacuolated cells. Reactive lesions may be seen at the
alveolar levels. These include necrosis of type I pneumocytes, alveolar
fibrosis, and a variable degree of type II pneumocyte transformation. Furthermore,
alveolar emphysema with an increase in Kohns`pores can be present. These
structural changes may explain the loss of lung compliance in horses with
severe RAO.
Whether
there is no causal relation between RAO and IAD that is not yet established. In both disorders, however, a poor climate in the stables plays
a role. It could be theoretisized that IAD eventually may result in RAO,
but there is no direct relation between IAD and RAO. In RAO
the hyperreactivity induced by histamine nebulization or to air allergens is
manifold more severe than in IAD, where only a mild bronchial hyperreactivity
often can be shown.
Since long time, based on observations made on members of generations of horse families, it was believed that RAO has a hereditary component. Just recently provided very strong evidence of an inherited predisposition to RAO on the basis of findings in two groups of horses. The same research group could demonstrate that mucin genes are likely to play a role too and that the IL4RA gene located on chromosome 13 is a candidate for RAO predisposition.
The results gathered so far suggest that RAO seems to be a polygenic disease.
Using segregation analysis for the hereditary aspects of the pulmonary health
status for two stallion families. A major gene plays a role in RAO. The mode of
inheritance in one family was autosomal dominant, whereas in the other horse
family RAO seems to be inherited in an autosomal recessive mode.
Refernces-
- Den Hoven, R. van. (2011). Air Pollution and Domestic Animals. Air Pollution - New Developments. doi:10.5772/17753.
- Wood, J.L.N., Newton, J.R., Chanter, N. & Mumford, J.A (2005). Association between respiratory disease and bacterial and viral infections in British racehorses. Journal of Clinical Microbiologyl, Vol. 43, pp. 120-126.
- Vandenput, S., Istasse, L., Nicks, B.,& Lekeux, P. (1997). Airborne dust and aeroallergen concentrations in different sources of feed and bedding for horses. Veterinary Quarterly, Vol. 19, pp. 154-158.
- Hayes, H.M. Jr, Hoover, R. & Tarone, R.E. (1981). Bladder cancer in pet dogs: a sentinel for environmental cancer? American Journal of Epidemiology, Vol. 114, pp. 229-233.


0 Comments